The Effect on Knowledge and Attitude of an Interprofessional Education Curriculum for Optometry and Physician Assistant Students
Raymond Chu, OD, MS
Abstract
The World Health Organization defines interprofessional education (IPE) as occurring when students from two or more disciplines learn with, from and about each other in order to prepare them for interprofessional collaborative practice (IPC).1 Due to the heterogeneous delivery of IPE, no consensus has been reached on the optimal number of course hours or instructional activities.2 As a result, there is limited data validating learning outcomes related to changes in knowledge, attitude and behavior. During the 2014-2015 academic year, students in the physician assistant and optometry programs at Marshall B. Ketchum University underwent an IPE curriculum. Survey comparison of pre-instruction and post-instruction showed no marked change in student readiness for IPC; however, the students’ knowledge of the roles of their counterparts increased. The lessons learned have helped further development of the IPE curriculum at Marshall B. Ketchum University.
Key Words: interprofessional education (IPE), interprofessional collaborative practice (IPC)
Background
The complexities of patient care have necessitated increased specialization within the U.S. healthcare system. This has created potential schisms in care as well as potential safety issues. Distinction among professionals has led to a lack of knowledge of the expertise of other health professionals and pre-conceptions and stereotyping that negatively affect collaborative practice. Pham et al. estimated that a typical Medicare physician coordinates with 229 other physicians in 117 different practices who also provide care to that same patient, yet communication errors between providers have resulted in poor patient outcomes.3,4 In response to the growing concern for the burden of care coordination, the American Academy of Family Physicians (AAFP), American Academy of Pediatrics (AAP), American College of Physicians (ACP) and American Osteopathic Association (AOA) issued a joint statement endorsing the concept of a “patient-centered medical home” where team-based care could be delivered effectively and efficiently in the interest of better patient outcomes and reducing healthcare cost.5
The World Health Organization and the Institute of Medicine have advocated to health profession programs to make interprofessional education (IPE) a priority in order to cultivate a collaborative, practice-ready workforce that is able to meet the call for team-based care.6,7 IPE aims to encourage students from different professions to work with one another in meaningful interactive learning activities that target the four core competency domains for interprofessional collaborative practice (IPC): 1) values/ethics for interprofessional practice, 2) roles/responsibilities, 3) interprofessional communication, and 4) teams and teamwork.8 Values and ethics for interprofessional practice reflect the common interests of providers working together to deliver safer, more efficient and more cost-effective care. Roles and responsibilities reflect how providers understand their role as well as the role of other team members. Interprofessional communication, where information is presented to all team members in an understandable manner, is crucial for effective interprofessional collaboration. Teams and teamwork reflect the need for providers to work together to reduce gaps and redundancies as well as share responsibility for problem-solving and decision-making.
The educational effectiveness of key elements of IPE has not been well-established because of the varied lengths of instruction and teaching methodologies.2 It is common for students from different health professions to attend the same course; however, some have argued that this is not truly IPE because of the limited opportunities for interaction among students.9 To foster participant engagement, some programs have employed problem-based learning or case-based learning, which have been helpful in developing the knowledge and behavior related to working in an interdisciplinary team.10 Institutions implementing IPE courses within their diverse health programs have commented that providing interprofessional learning experiences is a logistical challenge. Finding congruent times and locations to have students meet for IPE courses, meeting space conducive for small group discussions, and faculty modeling the desired behaviors are all challenges for an institution to address. Some have also suggested that meaningful collaboration can only occur when students have an adequate foundation regarding their own roles as healthcare providers. This would suggest that introduction of IPE should occur later in the curriculum as opposed to earlier. However, IPE curriculum introduced later in a professional program may not be as well-received because stereotypes and biases have already been formed.11 General consensus is that an IPE curriculum is best received when introduced early and with regular intervals of interaction.8,11
During the 2014-2015 academic year, Marshall B. Ketchum University delivered an IPE curriculum to its optometry and physician assistant students. The purpose of this study was to determine whether the IPE curriculum changed students’ readiness for interprofessional collaboration and their knowledge of each other’s roles within a healthcare team.
Methods
Interprofessional curriculum
In 2013, Marshall B. Ketchum University became home to the Southern California College of Optometry (SCCO) and the School of Physician Assistant Studies. The university identified coursework common to SCCO and the School of Physician Assistant Studies that could foster mutual respect between students from each program, help them to develop the communication skills for working as part of an interprofessional healthcare team, and provide knowledge about the role of the other provider.
The School of Physician Assistant Studies offers a 27-month (nine quarters) program with the bulk of didactic instruction during the first year followed by 12 six-week external clinical rotations. Conversely SCCO offers a four-year program (14 quarters) with the bulk of didactic instruction during the first three years and the final year focused on direct patient care in various clinics and health centers. Didactic courses were selected based on common coursework between the two professions. In the fall quarter, first-year optometry students and first-year physician assistant students were enrolled in the Professional Ethics course. In the winter quarter, second-year optometry students and first-year physician assistant students were enrolled in the Evidenced-Based Practice course. In the spring quarter, third-year optometry students and first-year physician assistant students participated in an interprofessional case-based conference.
In the Professional Ethics course, multidisciplinary faculty lectured weekly for one hour, which was followed by a one-hour small group (eight optometry and two physician assistant students with one faculty facilitator) case discussion. Topics such as Health Information Portability and Accountability Act, medical mistakes, errors in medical billing, and professional dishonesty were covered in the course and addressed using case-based learning in the discussions. Case-based learning utilizes a guided inquiry approach in which students are required to prepare ahead of the discussion in order to be a “content expert” so that meaningful dialogue can occur.
The Evidenced- Based Practice course was a lecture-based course taught by multidisciplinary faculty. Physician assistant and optometry students attended a weekly two-hour lecture with faculty presenting topics such as critical appraisal of the literature, application of evidence to clinical practice, and case studies of health outcomes as a result of interprofessional care.
In the interprofessional case-based conference, optometry and physician assistant students sat together at round tables with 8-10 students per table. A multidisciplinary team of faculty facilitators aided the one-hour discussion of the management of a poorly controlled diabetic patient. Portions of the case were presented with prompting questions within the table discussions. Representatives from each table, from both the optometry and physician assistant programs, were later asked to contribute to the large group discussion.
The cumulative experience for the physician assistant students was the opportunity to see the progression of learning of the optometry students (from first through third year) over the course of their one year of didactic instruction. Although the cumulative experience for optometry students was incomplete during this one-year study, first-year optometry students will eventually witness the progression of learning of the physician assistant students across the next three years of didactic instruction.
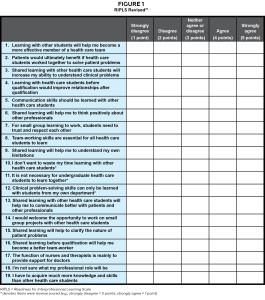
Readiness for Interprofessional Learning Scale (RIPLS)
The Readiness for Interprofessional Learning Scale (RIPLS) survey was selected for this study because of its ability to evaluate student attitude and perception of IPE as well as its widespread use within research relating to IPE. The RIPLS survey was originally published by Parsell and Bligh and was revised by McFadyen, Webster and Maclaren (Figure 1).12,13 The RIPLS survey is a validated survey consisting of 19 questions used to measure student attitude towards: teamwork and collaboration (Items 1-9), negative professional identity (Items 10-12), positive professional identity (Items 13-16), and roles and responsibilities (Items 17-19). Items within the teamwork and collaboration subscale reflect student attitude towards cooperative learning and mutual respect for one another. A higher score implies that students value those qualities. Items within the negative professional identity subscale relate to stereotypes and biases. These items were reverse scored (e.g., Strongly Disagree = 5, Strongly Agree = 1) so that a higher score implies that students value the opportunity for cooperative learning. Items within the positive professional identity subscale relate to students’ desire to improve communication and team skills, and a high score implies they value these shared learning experiences. Items within the roles and responsibilities subscale relate to students’ own roles. A high score implies an unclear perception of their role within the team.
During the 2014-2015 academic year university orientation, prior to the start of didactic instruction, first year students in both programs were administered the RIPLS survey. In addition to the RIPLS survey, knowledge of the role/responsibility of the counterpart profession was evaluated using a survey asking the following open-ended questions:
1. Identify 5 (or as many as you can) unique occupational duties of the counterpart profession. (For optometry students, identify duties of a physician assistant; for physician assistant students, identify duties of an optometrist)
2. What is the entry level of education needed to practice the counterpart profession?
3a. For physician assistant students: What is the difference between an optician, optometrist, and ophthalmologist?
3b. For optometry students: What is the difference between a nurse, nurse practitioner, physician assistant, and physician?
At the end of the 2014-2015 academic year, first-year students from both programs were re-administered the same surveys. In order to maximize participation, all participants were entered into a drawing for two $100 gift cards to Amazon.com. An application was submitted to the Institutional Review Board at Marshall B. Ketchum University, and the research was found to be exempt due to the anonymity of the surveys.
Statistical methods
A work-study student compiled the results of the two surveys into a Microsoft Excel spreadsheet. Items 10 through 12, which deal with negative professional identity, were reverse scored. Responses to the open-ended questions were classified for their accuracy based on the Occupational Outlook Handbook from the Bureau of Labor Statistics.14,15 Excel was used to calculate the mean and standard deviation within the sample for the two surveys. Due to the anonymous nature of the survey responses and the unequal number of participants within the optometry student responses, an unpaired t-test was used to evaluate the statistical significance between the pre-instruction and post-instruction RIPLS survey results.
Results
During the initial administration of the RIPLS survey and the survey on roles/responsibilities, 99 (99%) optometry students and 28 (100%) physician assistant students responded. During the re-administration of the surveys at the conclusion of the academic year, 92 (93.8%) optometry students and 28 (100%) physician assistant students responded.
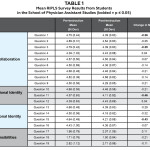
The results of the two administrations of the RIPLS survey are reported in Table 1 for the physician assistant students. Prior to IPE instruction, physician assistant students generally considered themselves ready for IPC. As a result of the IPE instruction, physician assistant students demonstrated a statistically significant decrease (p ≤0.05) in their readiness for IPC in two of nine questions within the teamwork and collaboration subscale, one of three questions in the negative professional identity subscale, and one of four questions in the positive professional identity subscale. The other 15 items within the RIPLS survey did not reflect a statistically significant change from pre-instruction to post-instruction.
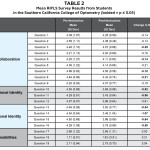
The results of the two administrations of the RIPLS survey are reported in Table 2 for the optometry students. Prior to IPE instruction, optometry students also considered themselves generally ready for IPC. As a result of the IPE instruction, optometry students showed a statistically significant decrease (p ≤0.05) in four of nine questions within the teamwork and collaboration subscale, two of three questions in the negative professional identity subscale, and four of four questions in the positive professional identity subscale. The other nine items within the RIPLS survey did not reflect a statistically significant change from pre-instruction to post-instruction.
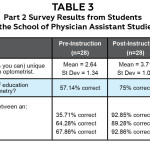
With respect to understanding one another’s roles and responsibilities, each student population was asked to identify the occupational duties of the counterpart profession (Tables 3 and 4). As noted in Table 3, the physician assistant student cohort demonstrated an improvement in understanding of one additional job responsibility by the end of the academic year and a 17.86% increase in correctly identifying the entry level of education. At the end of the academic year, physician assistant students also showed an increased ability to correctly differentiate between the role of an optometrist (+25% change), optician (+57.14% change) and ophthalmologist (+25% change).
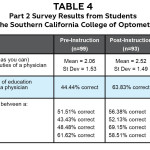
As noted in Table 4, the optometry student cohort demonstrated an improvement in understanding of 0.45 additional job responsibilities by the end of the academic year and a 19.38% increase in correctly identifying the entry level of education. At the end of the academic year, optometry students showed an increased ability to correctly differentiate between the role of a nurse (+4.87% change), nurse practitioner (+8.69% change) and physician assistant (+20.66% change) but a reduced ability to differentiate the role of the physician (-3.10% change).
Discussion
Kirkpatrick proposed a four-tiered framework for assessing learning outcomes in IPE: 1) learners’ reactions: learners’ view on the learning experience, 2) acquisition of learning: changes in knowledge, skills, competencies and attitude, 3) behavioral changes: the transfer of learning into workplace behavior, and 4) changes in organizational practice/changes to the organization.16 Assessing learners’ reaction to an IPE curriculum is a commonly employed outcome assessment of IPE. The results of our study were similar to the experience at Salus University where students’ self-perception of their readiness to practice in an interprofessional collaborative setting entered at a high level and continued to remain high after instruction.17 Although the results of the RIPLS survey showed statistically significant changes in some of the subscale items, the IPE curriculum is interpreted to have had no impact on student readiness for IPC. The limitation in this survey study was that measuring the impact of the IPE curriculum for the optometry students is premature due to their limited exposure of one course. At the time of the post-instruction survey, the optometry students had only taken one course with a lapse in time of about six months from the end of the course to post-instruction survey administration. Assessment of the impact of the IPE curriculum for optometry students will be more meaningful when the first-year optometry cohort completes its third and fourth years of study.
Most validated instruments for evaluating knowledge, skills and abilities focus on the knowledge of the instructor to deliver an interprofessional curriculum or evaluation of students’ abilities through interview or observations of clinical care teams. Assessment of IPE outcomes often does not assess knowledge acquisition about other professions. The open-ended questions used in this study were an attempt to assess a change in students’ knowledge of roles and responsibilities. Based on the results of the study, the IPE curriculum was able to increase students’ knowledge of the professional roles and responsibilities of those they were learning with.
Barr described the outcome of IPE as having three main themes: 1) preparing students for collaborative practice, 2) learning to work in teams, and 3) rendering services within an interdisciplinary team to improve care.18 Bridges et al. described the IPE training model at three universities in which the curricula included three common components: 1) a didactic program, 2) interprofessional simulation experience, and 3) a community-based experience.19 Thus, to prepare students with the knowledge, attitude and behavior for interprofessional collaborative practice, an IPE curriculum needs to include more than shared classroom experiences. It should also provide hands-on clinical opportunities within patient simulation and actual patient care.21
Conclusion
Best practices and key features of IPE for training health professionals to work together effectively are not yet established. Even less established is the understanding by other providers of the role of an optometrist in contributing to an interprofessional collaborative team.21 Marshall B. Ketchum University continues to refine its IPE curriculum with a focus on applying the lessons learned from the first iteration of the didactic curriculum and the additional focus of seeking IPE opportunities within co-curricular activities and culminating clinical experiences in model IPC settings.22
Acknowledgement
The research for this paper was supported by a Starter Grant for Educational Research from the Association of Schools and Colleges of Optometry. Funding for the grant was provided by Johnson & Johnson Vision Care, Inc.
References
1. World Health Organization. Framework for Action on Interprofessional Education & Collaborative Practice. Geneva Switzerland: WHO Press; 2010. https://whqlibdoc.who.int/hq/2010/WHO_HRH_HPN_10.3_eng.pdf?ua=1.
2. Reeves S, Zwarenstein M, Goldman J, et al. Interprofessional education: effects on professional practice and health care outcomes. In: The Cochrane Collaboration, ed. Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons, Ltd; 2008. https://doi.wiley.com/10.1002/14651858.CD002213.pub2. Accessed April 8, 2014.
3. Pham HH, O’Malley AS, Bach PB, Saiontz-Martinez C, Schrag D. Primary care physicians’ links to other physicians through Medicare patients: the scope of care coordination. Ann Intern Med. 2009;150(4):236-242.
4. Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186-194.
5. American Academy of Pediatrics (AAP), American College of Physicians (ACP), American Osteopathic Association (AOA), American Osteopathic Associatioin. Joint Principles of the Patient-Centered Medical Home. Washington D.C.: Patient Centered Primary Care Collaborative; 2007. https://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf.
6. WHO Study Group on Multiprofessional Education of Health Personnel. Learning Together to Work Together for Health: Report of a WHO Study Group on Multiprofessional Education of Health Personnel: The Team Approach. Geneva: World Health Organization; 1988.
7. Institute of Medicine (U.S.). Health Professions Education: A Bridge to Quality. (Greiner A, Knebel E, eds.). Washington, D.C: National Academies Press; 2003.
8. Schmitt M. Core Competencies for Interprofessional Collaborative Practice; 2011. https://www.aacn.nche.edu/education-resources/ipecreport.pdf.
9. O’Halloran C, Hean S, Humphris D, Macleod-Clark J. Developing common learning: the new generation project undergraduate curriculum model. J Interprof Care. 2006;20(1):12-28. doi:10.1080/13561820500471854.
10. Freeth D, ed. Effective Interprofessional Education: Development, Delivery and Evaluation. Oxford ; Malden, MA: Blackwell Pub; 2005.
11. Hind M, Norman I, Cooper S, et al. Interprofessional perceptions of health care students. J Interprof Care. 2003;17(1):21-34.
12. Parsell G, Bligh J. The development of a questionnaire to assess the readiness of health care students for interprofessional learning (RIPLS). Med Educ. 1999;33(2):95-100.
13. McFadyen AK, Webster VS, Maclaren WM. The test-retest reliability of a revised version of the Readiness for Interprofessional Learning Scale (RIPLS). J Interprof Care. 2006;20(6):633-639. doi:10.1080/13561820600991181.
14. Bureau of Labor Statistics. U.S. Department of Labor. Occupational Outlook Handbook, 2014-15 Edition, Physician Assistants. https://www.bls.gov/ooh/healthcare/physician-assistants.htm. Accessed September 11, 2015.
15. Bureau of Labor Statistics. U.S. Department of Labor. Occupational Outlook Handbook, 2014-15 Edition, Optometrists. https://www.bls.gov/ooh/healthcare/optometrists.htm. Accessed September 11, 2015.
16. Kirkpatrick DL. Evaluating Training Programs: The Four Levels. 3rd ed. San Francisco, CA: Berrett-Koehler; 2005.
17. Aravamudhan R, Vitek M, Casser L. The implementation and assessment of an interprofessional education initiative at Salus University. Optometric Education. 2015;40(3):11-15.
18. Barr H, ed. Effective Interprofessional Education: Argument, Assumption, and Evidence. Oxford ; Malden, Mass: Blackwell Pub; 2005.
19. Bridges DR, Davidson RA, Odegard PS, Maki IV, Tomkowiak J. Interprofessional collaboration: three best practice models of interprofessional education. Med Educ Online. 2011;16. doi:10.3402/meo.v16i0.6035.
20. Miller GE. The assessment of clinical skills/competence/performance. Acad Med. 1990;65(9 Suppl):S63-S67.
21. D’Amour D, Oandasan I. Interprofessionality as the field of interprofessional practice and interprofessional education: an emerging concept. J Interprof Care. 2005;19 Suppl 1:8-20. doi:10.1080/13561820500081604.
22. Hammick M, Freeth D, Koppel I, Reeves S, Barr H. A best evidence systematic review of interprofessional education: BEME Guide no. 9. Med Teach. 2007;29(8):735-751. doi:10.1080/01421590701682576.