The Implementation and Assessment of an Interprofessional Education Initiative at Salus University
Radhika Aravamudhan, PhD, CCC-A, FAAA, Melissa Vitek, OD, FAAO, Linda Casser, OD, FAAO, FNAP
Abstract
This paper describes a pilot project designed to assess student perceptions and attitudes in the context of interprofessional education (IPE) clinical problem-solving (CPS) sessions. Participants were first- and second-year student volunteers from the optometry, audiology and physician assistant programs at Salus University. Perceptions and attitudes toward the IPE learning environment were assessed utilizing standardized questionnaires. The pre- and post-session scores were compared using t-tests to evaluate change in perceptions and attitudes after the IPE-CPS sessions. The results of this pilot project will assist in the design, implementation and outcome measurement of future IPE offerings at Salus University.
Key Words: interprofessional education, interprofessional practice, teamwork, clinical problem-solving
Background
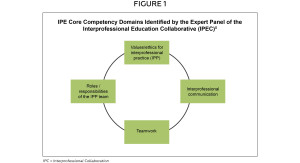
Precipitated by the evolving healthcare environment over the past decades, interprofessional education (IPE) and interprofessional practice (IPP) have gained increased prominence in professional education.1,2 The Centre for the Advancement of Interprofessional Education defines IPE as occurring “when two or more professions learn with, from and about each other to improve collaboration and the quality of care.”3 As a result, student interaction has become a defining feature of both IPE and IPP.4 A group comprised of leaders from the national organizations of six healthcare professions, the Interprofessional Education Collaborative Expert Panel, has identified four IPE core competency domains that all healthcare professions should include in their educational curricula.5 (Figure 1) A World Health Organization study group on Interprofessional Education and Collaborative Practice defined learning objectives for IPE. The six competencies defined are: teamwork, roles/responsibilities, communication, learning/reflection, ethics/attitudes and the patient.6 The quantity, quality, environmental factors and ultimate goals of student interaction in this context have been the subject of many publications. Specifically, surveys have been utilized to measure the impact of interprofessional interaction on student perceptions and attitudes. While there is broad agreement on the importance of enhancing teamwork, there remains little consensus on how to most appropriately measure it.7 Parsell and Bligh developed a questionnaire and associated Readiness for Interprofessional Learning Scale, which includes subscales.8 The teamwork and collaboration subscale measures students’ beliefs about the benefits of shared learning, and the professional identity subscale focuses on assessing role relationships and professional identity.6 McFayden and Maclaren developed the Interdisciplinary Education Perception Scale, which measures how students perceive their profession.9 The University of West England developed an Interprofessional Questionnaire to evaluate teamwork and communication skills.10 All three measurement tools were utilized in this IPE-CPS pilot study.
Salus University, named for a Latin word meaning health and well-being, is a diversified, globally recognized, professional academic center of learning that offers a wide range of accredited postgraduate degree programs in optometry, audiology, physician assistant studies, public health, education and rehabilitation of the blind and visually impaired, biomedicine, occupational therapy and speech-language pathology (anticipated launch in 2015). In September 2012, the Salus University Office of Academic Affairs established the Salus University Interprofessional Education Committee comprised of representatives from all on-campus colleges. The Salus University IPE Committee facilitated the development and launch of an IPE-CPS pilot, which was launched early in 2014. The pilot program involved students from the optometry, audiology and physician assistant programs. These students were chosen because the core didactic curricula of their respective programs include CPS courses. The format of these courses emphasizes small group case-based or problem-based learning. This learning setting provides an opportunity for students to synthesize and apply the theoretical and practical aspects of critical thinking in the process of clinical problem-solving — history-taking, diagnostic data collection, patient assessment and patient management — utilizing prepared clinical cases. An important additional goal of the CPS courses is to effectively serve as an integrated educational bridge between the didactic and clinical courses within a health professions curriculum. Selecting this type of small group-based activity for this IPE initiative was important due to the interactive nature of the CPS environment.
Prior to this pilot study, Salus’ first-year students in optometry, audiology and physician assistant studies had an opportunity to work in IPE teams in their fall semester core curriculum Evidence-Based Practice course, while the second-year students did not have a similar opportunity. Thus, this pilot project compares data from two student cohorts, first- and second-year students, who had different IPE experiences in their respective core curricula prior to the pilot.
The purpose of this IPE-CPS pilot was to investigate the following:
1) Does exposure to IPE increase student understanding of other healthcare professions?
2) Do the standardized questionnaires utilized in this study to assess IPE perceptions and attitudes deliver meaningful information?
3) Does early exposure to IPE increase student understanding of the significance of IPE environments?
Methods
Participant recruitment
Following Institutional Review Board approval, student participants from the optometry, audiology and physician assistant programs were recruited via e-mail announcements on a first-come basis. Students provided signed informed consent to participate in this five-week IPE-CPS pilot study. These specific professions were chosen to participate in the study because their educational programs at Salus University have CPS courses as a component of their core curricula.
This study was conducted utilizing two cohorts, one comprised of first-year students (n=9) and the other of the second-year students in the aforementioned professional programs (n=10). Because the first-year students had previous exposure to IPE teamwork in their fall term as a part of their Evidence-Based Practice course that was modified for this cohort to include team-based work, while the second-year students did not, students participated in the IPE-CPS sessions as two separate cohorts. This study was conducted in the spring term for both cohorts and these were student volunteers.
Study design and data analysis
The study used a mixed-methods approach involving pre- and post-questionnaires and qualitative comments to gain a deeper understanding from the students about their experience in the IPE-CPS pilot project. The study evaluated students’ attitudes relative to interprofessional collaboration before and after exposure to the IPE-CPS experience. The pre-experience and post-experience mean scores were compared using a parametric analysis with t-test to evaluate whether there was a significant difference within and/or between cohorts (p<0.001).
IPE-CPS session format
A modified problem-based learning approach was utilized to facilitate the IPE-CPS sessions. A case of a patient diagnosed with type 2 diabetes mellitus was chosen for this study because of the relevance of this disease to all of the three participating professions. The IPE-CPS sessions were conducted for five weeks. Each cohort met for two hours per week in the evenings with three faculty facilitators. Faculty members from Salus University’s audiology, optometry, physician assistant and public health programs served as the facilitators. The goal was to ensure that at least one faculty member from each program was involved to cover discipline-specific content areas of the patient case.
Weeks 1 and 2: Pre-assessments were performed utilizing three standardized IPE questionnaires. Following the pre-assessments, the patient case details were presented by the facilitator in a problem-based learning format such that the information about the case was presented as the students requested the information. Weeks 1 and 2 focused on discussions surrounding the diagnosis of the patient case.
Weeks 3 and 4: The discussions and facilitation were focused on the interprofessional management, treatment and rehabilitation of the patient case.
Week 5: The discussions and facilitation were focused on generalizing the recommendations for this patient case to a population, including how the results from this patient case relate to public health. Post- assessments were conducted utilizing three standardized IPE questionnaires.
Questionnaires
In order to assess the student impact of interprofessional education, the following questionnaires were utilized to evaluate student perceptions, values and attitudes toward IPE: 1) the Readiness for Interprofessional Learning Scale (RIPLS),8 2) the Interdisciplinary Education Perception Scale (IEPS),9 and 3) the University of West England Interprofessional Questionnaire (UWE-IPQ).10 These survey tools were used in this pilot project because the validity and reliability of all three questionnaires have been established.8,9,10
Results
Quantitative Findings
Pre-post comparisons of the UWE-IPQ mean scores
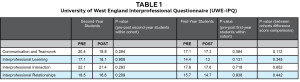
Table 1 represents the mean scores and p values for the UWE-IP questionnaire. The questionnaire is divided into four categories:
Click image to enlarge
Mean scores for each category utilizing the University of West England Interprofessional Questionnaire. Scores interpretation: None of the differences was statistically significant between pre and post based on the p values. Communication and Teamwork: 9-20 (Positive) 21-25 (Neutral) and 26-36 (Negative); Interprofessional Learning: 9-22 (Positive) 23-31 (Neutral) and 32-45 (Negative); Interprofessional Interaction: 9-22 (Positive) 23-31 (Neutral) and 32-45 (Negative); Interprofessional relationship: 8-20 (Positive) 21-27 (Neutral) and 28-40 (Negative).
communication and teamwork; interprofessional learning; interprofessional interaction; and interprofessional relationships.
Within cohort comparisons: A paired t-test was applied for each category to both cohorts separately for pre- and post-scores to test for significance, and none of the differences was found to be statistically significant.
Between cohort comparisons: The mean difference between the pre- and post-scores of the two cohorts was compared using a t-test, and none of the categories showed any significant difference between the two cohorts.
Pre-post comparisons of the IEPS mean scores
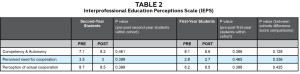
Table 2 presents the mean scores and p values obtained on each of the categories represented in the IEPS questionnaire. This questionnaire is divided into three categories: competency and autonomy; perceived need for cooperation; and perception of actual cooperation. Both within and between cohort comparisons failed to show any significant differences (p<0.001).
Click image to enlarge
Mean scores in each of the areas from the Interdisciplinary Education Perception Scale. Scores Interpretation: None of the differences was statistically significant based on the p values.
Competency and Autonomy: 7-9 mean scores=strongly agree/agree (positive perception); Perceived Need for Cooperation: 2-4 mean scores=strongly agree/agree (positive perception); Perception of Actual Cooperation: 6-12 mean scores=strongly agree/agree (positive perception).
Pre-post comparisons of RIPLS mean scores
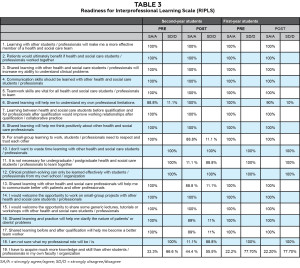
Table 3 represents the mean percentage response for each question on the RIPLS questionnaire. Each of the 100% mean scores represents a strong positive perception of the IPE learning environment.
Even though there was no significant difference between the pre- and post-survey data, the overall data as well as the qualitative student comments (below) confirmed a positive student perception and understanding of both the need and value of interprofessional education. The results indicate that the students entered the study with a positive attitude toward the significance of IPE and concluded the study with the same positive perception.
Qualitative student comments
• “I learned a lot more about other professions.”
• “I loved thinking with students from other professions.”
• “This experience motivated me to research areas that I did not know a lot about and may not have done it on my own if not for this project.”
• “I learned how important co-management is to patients.”
• “I learned that I do not need to know everything.”
• “An excellent learning experience that allowed personal growth in a challenging, engaging and exciting environment.”
• “I benefited greatly by gaining insight into the decision-making process of those from the other professions.”
Discussion
The data collected in our pilot study indicate strong positive attitudes, perception of, and need for interprofessional education among the students participating in this study. However, there are limitations to the data collected. There was no statistically significant difference between the pre- and post-survey data within each cohort. This could be due to several factors including the small sample size and the fact that participants were
Click image to enlarge
Mean percentages obtained from the Readiness for Interprofessional Learning Scale.
student volunteers. Student volunteers are inherently more likely to have a positive attitude toward interprofessional team work.11 The outcome shown by the data could also be due to limitations in the surveys utilized in the data collection. It is possible that the questions included in the surveys do not include a level of specificity needed to adequately quantify small differences between students and/or small changes within students. The UEW-IPQ reversed the response ratings in between categories, which may have confused some of the participants. Using a similar rating scale throughout may have facilitated consistent ratings from the participants.
Early IPE exposure is thought to diminish the development of negative stereotypes and positively impact the development of positive professional attitudes.11 Therefore, it was anticipated that the first-year students’ exposure to IPE teamwork in the Evidence-Based Practice course would have resulted in a difference in their data when compared to the second-year students as the latter did not have similar prior experience. Specifically, it was expected that the first-year students would have higher pre-survey scores than the second-year students with regard to positive attitudes, values and perceptions. In addition, it was theorized that the post-survey data may also be higher in positive attitudes, values and perceptions as this cohort of students would be more experienced in an IPE setting. Again, the lack of difference between these cohorts may also be due to the small sample size as well as the fact that the student participants were all self-selected volunteers.4, 11
The qualitative student comments indicate that the IPE-CPS experience differed from their respective core curriculum CPS experiences in important ways. Specifically, it appears that the foundation for respectful interprofessional communication and effective co-management of patients is a promising potential outcome of IPE initiatives such as this IPE-CPS. Although evidence suggests that effective teamwork should provide patients with better outcomes, most studies conducted thus far do not directly measure the link between these two variables.7 The lessons learned from this pilot study regarding implementation and assessment will serve as a catalyst for future IPE and IPP initiatives at Salus University in which larger groups of students can participate and more meaningful data can be collected.
Conclusions
The health professions/provider community has recognized the critical importance of interprofessional education and practice, and has responded with a variety of initiatives, projects and events aimed at improving communication, addressing challenges and barriers, and improving the effectiveness of teams.12 Salus University students are learning to become members of health/rehabilitation teams, and they are getting to know each other for their discipline-specific knowledge and skills.
The data collected in this IPE-CPS pilot project indicated that the baseline level of student commitment to and readiness for IPE was high and remained high throughout the pilot project. Consistent with experiences on other campuses,1 the efforts and activities of the Salus University IPE Committee to date, including this pilot project, have fostered a very positive attitude toward IPE experience among participants that is undiminished at the time of post-test. Following the positive feedback from the participating students, we have continued to conduct volunteer IPE-CPS sessions to obtain a larger sample size and evaluate effectiveness.
Acknowledgements
We extend sincere thanks and appreciation to: Anthony Di Stefano, OD, MEd, MPH, for his leadership in naming the inaugural IPE Committee at Salus University while serving as Vice President of Academic Affairs; Anthony Di Stefano, OD, MEd, MPH, Joy Henderson, MMS, PA-C, Jonette Owen, AuD, and Thomas Lewis, OD, PhD, for serving as facilitators for this IPE-CPS project; and the Salus University students who participated and enthusiastically shared their suggestions: Alyssa Acquavita, Sofia Ahmad, Stephanie Borja, Christin DeMoss, Shelby Favre, Victoria Galbreth, Nicholas Karbach, Julia Kuksin, Lili Liang, Florencia Lopez, Britney Martin, Meghan Mahoney, Kalie McCartin, Erika Peavy, Daniel Situ, Alison Suktis, Bianca Tang, Kat Tribulski and Kristen Vincent.
References
1. Buring SM, Bhushan A, Brazeau G, Conway S, Hansen L, Westberg S. Keys to successful implementation of interprofessional education: learning location, faculty development, and curricular themes. Am J Pharm Educ. Interprofessional education supplement. 2009;73(4):Article 60.
2. Aston S, Rheault W, Arenson C, Tappert SK, Stoecker J, Orzoff J, Galitski H, Macintosh S. Interprofessional education: a review and analysis of programs from three academic health centers. Academic Medicine. 2012;87(7):949-955.
3. Center for the Advancement of Interprofessional Education (CAIPE) [Internet]. (Cited 2015, Jan 20). Available from: https://www.caipe.org.uk.
4. Eccott L, Greig A, Hall W, Lee M, Newton C, Wood V. Evaluating Students’ Perceptions of an Interprofessional Problem-Based Pilot Learning Project. Association of Schools of Allied Health Professions. 2012.
5. Formicola AJ, Andrieu SC, Buchanan JA, Childs GS, Gibbs M, Inglehart MR, Kalenderian E, Pyle MA, D’Abreu K, Evans L. Interprofessional education in US and Canadian dental schools: an ADEA Team Study Group Report. Journal of Dental Education. 2012;76(9):1250-68.
6. Ravet J. From interprofessional education to interprofessional practice: exploring the implementation gap. Professional Development in Education. 2012;38:1:49-64, DOI: 10.1080/19415257.2011.576263.
7. Havyer RDA, Wingo MT, Comfere NI, Nelson DR, Halvorsen AJ, McDonald FS, Reed DA. Teamwork assessment in internal medicine: a systematic review of validity evidence and outcomes. Journal of General Internal Medicine. December 2013;29(6):894-910. DOI: 10.1007/s11606-01-2686-8.
8. Parsell G, Bligh J. The development of a questionnaire to assess the readiness of health care students for interprofessional learning (RIPLS). Medical Education. 1999:33(2):95.
9. McFadyen AK, Maclaren WM, Webster VS. The Interdisciplinary Education Perception Scale (IEPS): an alternative remodeled subscale structure and its reliability. J Interprof Care. 2007;21(4):433-443.
10. Pollard K, Miers M, Gilchrist M. Second year scepticism: pre-qualifying health and social care students’ midpoint self-assessment, attitudes and perceptions concerning interprofessional learning and working. J Interprof Care. 2005:19(3):251-268.
11. Cusack T, O’Donoghue G, Butler M, Blake C, O’Sullivan C, Smith K, Sheridan A, O’Neil G. (2012) A pilot study to evaluate the introduction of an interprofessional problem-based learning module. Interdisciplinary Journal of Problem-Based Learning. 2012;6(2).
12. Kanter SL. Can we improve interprofessional team-based patient care without calling 9-1-1? Academic Medicine. 2012;87:253-254.
13. Hall LW, Zierler BK. Interprofessional education and practice guide no. 1; developing faculty to effectively facilitate interprofessional education. Journal of Interprofessional Care. J Interprof Care. 2015;29(1):3-7.