Hyperopia and Presbyopia: A Teaching Case Report
Nancy B. Carlson, OD, FAAO, and Aurora Denial, OD, FAAO
Abstract
This case report demonstrates the importance of doctor-patient communication. This patient, a fairly straightforward hyperopic presbyope, had a lot of anxiety about his symptoms and was very worried that he might have a dreadful disease, perhaps a brain tumor. The patient needed a supportive environment to express his concerns and empathetic clinicians to calm him down. Early in their training, students have difficulty focusing on patient communication because they are so concerned with gathering accurate data. Discussions about patients like the one presented here give the students opportunities to practice good patient communication skills.
Key Words: hyperopia, presbyopia, determining adds, OTC glasses, patient communication
Background
Presbyopia is an age-related refractive condition that results from the normal decrease in amplitude of accommodation necessitating a prescription of plus for near vision.1 Presbyopia is a common condition in patients over age 40 that most optometrists in practice encounter daily. The techniques for determining the appropriate near prescription for a presbyope are described in many optometric textbooks as well as in the American Optometric Association’s Clinical Practice Guideline on Care of the Patient with Presbyopia.2-9 Because optometry students typically practice on each other until they are assigned to clinic, they may fear that examining a presbyope will be very difficult when in fact the examination process is quite straightforward. One of the more difficult parts of the care of the presbyope is tailoring patient management to each individual patient’s needs and helping the patient to understand the changes in vision. Patient management can be challenging and takes good listening skills, experience, patience and finesse. While presbyopia is a normal consequence of aging and occurs in everyone sometime after age 40, many patients are surprised by its onset. This case illustrates the process of determining the prescription for the presbyope as well as the importance of giving the patient the empathy, care and support he needs as he begins to need near glasses and continues to see his vision and his correction changing. The case is appropriate for first-year students or for students who are just starting their clinical training. This case can also be used for third- or fourth-year students to review and reinforce the principles and techniques used in caring for presbyopic patients.
Student Discussion Guide
Case description
BD, a restaurant maître d’ and personal trainer, presented for an eye exam at age 52 complaining of blur at near both with and without the over-the-counter (OTC) readers he had been using for five or six years. He reported good vision at distance except for some difficulty driving at night. BD had never had an eye exam and he was very concerned that his vision might be deteriorating due to an underlying issue with his health. BD reported his general health as good. He had been taking 10 mg of lisinopril daily for hypertension for 20 years. His blood pressure had last been checked three months before his eye exam. He also reported seasonal allergies, and he was taking Flonase for nasal congestion as needed. He had no allergies to medications. Further personal and family history was unremarkable.
• Visual acuity at distance without correction
OD 20/25
OS 20/80 PH 20/40
• Visual acuity at near without correction
OD 20/80
OS 20/120
• Entrance tests (color vision, cover test, Randot 2, NPC, EOMs, pupils, screening visual fields)
normal
• Retinoscopy
OD +1.50
OS +2.50
• Distance subjective refraction
OD +1.00 20/20
OS +2.00 20/20
• NRA/PRA through a tentative add of +2.00 (tentative add based on the patient’s age)
+1.50/-1.50
The distance subjective refraction was trial framed, and BD noted that things looked clear and comfortable at distance looking not only at the Snellen chart but also down the hall from the clinic and out the window at cars in the parking lot. The add of +2.00 (net near Rx was OD +3.00 and OS +4.00) was trial framed over the distance Rx, and BD found that his vision was much improved from his OTC readers of +2.00. BD’s range of clear vision through the trial-framed add was 10” – 20”. In the initial case history, BD did not inform the clinician about his OTC glasses. It was not until BD became comfortable with the clinician that he reported that he had been using readers for several years. Because they were not prescribed, he did not think of his readers as “glasses” and he was somewhat embarrassed to admit to using them. BD said, “Oh, these are not glasses, they just magnify things so I can see them.”
BD’s Goldmann tonometry readings were OD 14 mmHg and OS 14 mmHg at 2:10 p.m. He was dilated with one drop of 1% tropicamide and one drop of 2.5% phenylephrine in each eye. The dilated fundus exam with the binocular indirect ophthalmoscope and 78D lens and slit lamp was normal.
Progressive addition lenses with an Rx of OD +1.00 OS +2.00 Add +2.00 were recommended. BD was also told that although he primarily needed glasses for near work, the prescription given would also be useful for distance, especially for driving at night. He was advised that he could use the glasses for near and still see clearly at distance. As an alternative, he could wear them full-time. For his job as a maître d’, wearing the glasses all the time would be most practical. For his job as a personal trainer, he might prefer to put the glasses on only for near tasks. BD was instructed to return for a comprehensive exam in one year.
The patient education for BD included a description of presbyopia as a normal change in vision due to age and that his eye exam did not reveal any evidence of ocular or systemic disease. BD was also told that it was expected that he would need to wear his glasses more frequently as he continued to age and that it was expected that the prescription would need to be changed over time. As he was leaving the clinic, BD expressed his appreciation for the demonstration of his new prescription and for the explanation of presbyopia. He was told to call if he had any questions about his eyes, his vision or his glasses.
About a week after he received his glasses, BD called and said, “You’ve ruined my life!” He went on to explain that he thought his apartment was clean but now that he had glasses, he could see that it was not and he had a lot to do to clean it up. He said he had thought he was functioning fine with just his OTC readers, and now he was finding himself wearing the progressive addition lenses almost all the time. He found that he liked clear, comfortable vision much more than blurry vision. He again expressed appreciation for his improved vision and said he looked forward to his next exam.
Despite reminders by mail and phone, BD did not return for an examination for three years. He made several appointments over those years but canceled because he was too busy at his two jobs. When he finally made an appointment that he kept, he was very agitated because he could no longer see to read even wearing his glasses. He was again worried that his visual symptoms might mean that he had a terrible disease, perhaps even a brain tumor. BD also reported that he was having a difficult time at his job as a maître d’ because he could not see the menus or read the list of specials. He reported that his boss had threatened to fire him if his vision could not be improved.
BD’s medical history was unchanged from his previous visit. He was still taking 10 mg of lisinopril daily for high blood pressure. He reported that his last physical exam was one month previous and his doctor found no problems with his health but recommended that he have an eye examination.
• Visual acuity at distance with correction (OD +1.00 OS +2.00, add +2.00)
OD 20/200 PH 20/40
OS 20/60 PH 20/30
OU 20/70
• Visual acuity at near through the add
OD 20/120
OS 20/120
OU 20/120
• Entrance tests (color vision, EOMs, Pupils, screening visual fields)
normal
• Retinosocpy
OD +1.50
OS +2.00
• Distance subjective refraction
OD +3.00 20/20
OS +3.25 20/20
• NRA/PRA through a tentative add of +2.75 over the distance subjective (add chosen based on the patient’s near visual acuity through his old glasses)
+1.00/-1.00
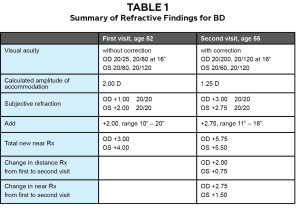
The distance subjective refraction was trial framed, and BD noted that things looked clear and comfortable at distance, but he preferred +0.50 less in his left eye. He reported that his vision was much improved from his previous glasses. An add of +2.50 and an add of +2.75 were trial framed over the adjusted distance Rx. BD preferred the add of +2.75. He also reported that the new prescription improved his vision greatly at near compared to his previous Rx. His range of 11” to 18” was adequate for his visual needs. An Rx of OD +3.00 and OS +2.75 with an add of +2.75 was recommended. See Table 1 for a summary of the refractive data for BD’s two examinations.
Goldmann tonometry was OD 12 mmHg, OS 12 mmHg. The patient was again dilated with one drop of 1.0% tropicamide and one drop of 2.5% phenylephrine in each eye. The dilated fundus exam was normal.
Although BD could see that his vision was improved to 20/20 in each eye at both distance and near, he expressed that he was very concerned with the large change in his vision and his prescription over a period of three years. He asked again if this was due to a disease and was reassured that it was a normal change. He was also advised that he could expect continued changes in his prescription in the years to come. He asked if his vision would change so much that glasses strong enough to correct his vision would not be available. BD was reassured that glasses would be available for him. He was advised to return for a comprehensive examination in one year.
Educational Guidelines
Key concepts
1. Correlation of visual acuity at distance and near to refractive findings
2. Natural history of hyperopia
3. Natural history of presbyopia
4. Testing used to determine a prescription for a hyperopic presbyope
5. The importance of patient education, especially for adults with their first prescription
6. The importance of empathizing with patients about their vision problems
Learning objectives
1. To identify and list the signs and symptoms of hyperopia and presbyopia
2. To be able to correlate symptoms with refractive findings
3. To describe the epidemiology of presbyopia
4. To describe the expected course of changes in hyperopia in adults and in presbyopia
5. To be able to describe the difference between an add and a near prescription
6. To be able to elicit an individual patient’s concerns about vision and respond to them appropriately
Discussion questions
A. Knowledge, Concepts, Facts, Information Required for Review of the Case:
1. Describe the signs and symptoms of hyperopia and how it manifests and changes as patients age
2. Describe the signs and symptoms of presbyopia
3. Describe the testing that is done to determine the appropriate prescription for a hyperopic presbyope
4. Describe the natural history of hyperopia
5. Describe the etiology and demographics of presbyopia
6. Describe the impact of a normal age-related reduction in amplitude of accommodation on visual acuity at distance and near for a hyperopic presbyope
7. Discuss the development of refractive amblyopia in anisometropic hyperopes who are uncorrected before the age of 6-8
8. Describe the options for correcting hyperopic presbyopia
9. Discuss the impact of hyperopic presbyopia on a patient’s life
10. Discuss the various reactions of patients to the diagnosis and treatment of hyperopic presbyopia, including surprise, anxiety, anger, relief, etc., and how to deal with these reactions
11. Discuss the most common ocular and systemic diseases that should be screened for in the presbyopic population
B. Generating Questions, Hypothesis and Diagnosis:
1. What tests were used to diagnose hyperopic presbyopia?
2. What was the differential diagnosis for the patient’s symptoms and how were the other hypotheses ruled out?
C. Management:
1. What are the options for treating hyperopic presbyopia?
2. What is the best option for this patient?
3. How do the patient’s jobs influence the recommendations for the best option for this patient and for the recommendations for wearing his prescription?
4. What patient education should be given to all hyperopic presbyopes?
5. Discuss this patient’s reaction to his symptoms and how it affects the patient education given and the communication with the patient throughout the examination.
Discussion Points
Before these examination results can be discussed, students should have basic knowledge about presbyopia: definition; epidemiology; etiology; onset and progression; procedures for testing, including methods for determining a tentative add, NRA/PRA, measuring the range and trial framing the prescription; optical options for correcting presbyopia; ocular and systemic health issues prevalent in the presbyopic population; and patient communication with presbyopes. Students may learn this information through lectures, readings, online resources or a combination of these learning methods. In addition, students should have a lab and practice the techniques used for determining a presbyopic prescription. If the students are testing each other in lab, the student serving as a patient can be cyclopleged with 1% tropicamide to simulate presbyopia.
Students can be given cases to review, such as those in Kurtz’s chapter in Brookman (1994),10 Ettinger and Rouse (1997)11 and Werner and Press (2002).4 Although these cases will be somewhat similar to the case presented here, repetition is a tried and true learning method that helps students to master material.
A faculty member, teaching assistant or student can lead a discussion of this case either in a large classroom setting or in a small group. Students should be given all of the history, clinical data and patient education from both visits to review before the case discussion. Students should be encouraged to write questions they have about the case along with a list of topics they would like to discuss.
The discussion can start with an analysis of the patient history. Given BD’s age and complaints, what do they expect to find during the examination? Because BD never had an eye examination before age 52, he is likely to be emmetropic or hyperopic. It is also likely that he has been presbyopic for several years. The epidemiology, etiology, onset and progression of presbyopia can also be discussed when analyzing the case history. When would BD have been first expected to have symptoms of presbyopia? How did he manage to be 52 before needing an eye exam? Is this common? Were his OTC glasses of +2.00 that he wore since approximately age 46 a large add for that age? How did his refractive error contribute to the prescription of plus that he needed for near? Review the difference between a near prescription and an add with the students. For BD, +2.00 OTC readers were most likely a partial correction of his hyperopia with an add. Patients in their 40s usually need a first add of +0.75 or +1.00, so BD’s glasses of +2.00 were likely to be +1.00 or +1.25 to correct hyperopia with an add of +1.00 or +0.75. When a patient is wearing +2.00 for near in his 40s, hyperopia is the expected refractive error.
Symptoms of presbyopia generally first occur in patients age 40 to 45.12 Many patients cope with the symptoms of blur at near by increasing light or moving reading material further away to decrease the demand on their accommodation. Often patients will resort to OTC plus lenses as a solution to their problem. As the amplitude of accommodation continues to decrease and patients notice the solutions are no longer working, they finally have an eye exam. Although optometrists are expecting to find presbyopia in their patients after age 40, Walline, Zadnik and Mutti13 (1996) found that more than half of the patients surveyed did not know the definition of presbyopia or how it would affect them in their activities of daily living.
BD did not reveal he was using OTC reading glasses until after the refraction. He was somewhat embarrassed by this. Discuss the patient’s perception that OTC readers are not “real glasses.” Is this a common perception? Would it be possible to elicit this information earlier in the exam or during the case history? Perhaps a question such as “What do you do when you are having trouble with close work to make it easier to see? Do you use more light, hold things further away or use glasses from the drugstore?” would help the patient to realize that some of the attempted solutions are not unusual.
Patient communication is obviously important in every patient encounter and, as Ettinger (1994) says, is “the core of good clinical care.”14 Students need to learn to make the patient the most important person in the room during the exam. They also need to develop good listening skills and empathy to let the patient fully express his or her concerns. In this case, BD had an extroverted personality and was fairly comfortable talking with the clinicians. He did, however, show anxiety about his “deteriorating vision” at both exams. Although presbyopia is inevitable, most patients do not know that fact and many are surprised and upset by the symptoms of presbyopia and what they mean.12 Discuss how to alleviate the patient’s concerns. What tests were done as part of this exam to rule out health problems as a cause for the patient’s symptoms? What else could have been said as part of the patient education that might have helped BD? Discuss the use of written materials for patients that explain common eye conditions.
Lloyd and Bor (2004)15 report that the goals of patient education include helping patients understand their conditions, reducing their anxiety and enlisting their cooperation in the management of the problem. BD’s follow-up call the week after he received his glasses seemed to demonstrate that he understood the problem at that time and could even laugh about it. Despite that, he had developed a lot of anxiety by the time of his second appointment three years later. Some of his anxiety was no doubt due to his hectic work schedule. At his second visit, he was obviously very relieved when he saw his vision improved to 20/20 at both distance and near with a change in prescription.
Is there anything in the initial case history that points to the possibility of an ocular or systemic health problem? What are the common health issues that should be screened for in a 52-year-old patient? Cataracts, glaucoma, high blood pressure and diabetes are most common in this age group and are screened for in every adult examination. Macular edema, thyroid abnormalities and orbital masses can cause refractive changes and should be considered when there are changes in visual acuity, color vision or refractive error.9,16 For BD, specific discussion of what testing was done and how it ruled out ocular and systemic disease would help to reassure him about his health. Werner and Werner17 (1979) emphasize the importance of showing sensitivity to the entire patient and not just his or her eyes. Many patients view presbyopia as another sign of aging, but don’t know that the amplitude of accommodation diminishes for many years before reading glasses are needed. It is often helpful to let patients know this.
Review the exam data. Is the uncorrected visual acuity at distance and near correlated with the subjective refraction and add findings? Based on the patient’s age, what add is expected? How does the distance refraction affect the add?
The hyperopic patient’s distance visual acuity without correction is related to the amount of hyperopia and the patient’s amplitude of accommodation. Patients are usually comfortable if they are using no more than half of their accommodation. During visual acuity measurement, a patient is able to use all of his accommodation to read a line of letters because it only takes a few seconds. In this case, BD at age 52 would be expected to have an amplitude of accommodation of 2.0 D according to Hofstetter’s formula: Amplitude of Accommodation = 15 – 0.25 X age. At his first visit, his distance uncorrected visual acuity was 20/25 in the right eye and 20/120 in the left eye. The subjective refraction showed +1.00 in the right eye and +2.00 in the left eye. Uncorrected distance visual acuity in hyperopes is not always as predictive of the refractive error as it is in myopes.
The initial refraction revealed a difference in hyperopia between the two eyes. Refractive amblyopia is not a concern for this patient since BD’s vision is correctable to 20/20 in each eye and he is well past the age of 6 to 8 when the development of amblyopia is a concern.18 However, if his vision was decreased in the eye with the higher hyperopia amblyopia versus pathology would have to be investigated.
The natural history of hyperopia is that it becomes more manifest as the patient ages, and the ability to compensate for it decreases with the normal decrease in amplitude of accommodation.19-21 Because BD had his first eye exam at age 52, there is no previous data to show how hyperopic he was at an earlier age. With many patients, the full amount of hyperopia is not known unless the patient has been cyclopleged or until the patient is presbyopic. Cycloplegic refraction is not indicated in a patient with an expected amplitude of accommodation of 2.0 D.
Discuss the options for correcting presbyopia. Why were progressive addition lenses recommended for BD? Does he need to wear them full-time? Is he likely to wear them full-time at this point? Given that his distance vision without correction was 20/25 at his first visit, it is unlikely that he will start wearing progressive addition lenses full-time. Because he has managed to function with OTC readers for several years, he will be quite likely to use his PALs in the same manner. Discuss how his jobs will determine his visual needs and his use of glasses. Many presbyopes wear contact lenses, which can be considered in the future for BD.
The assessment of the learning objectives can occur in several ways. In a clinical exam setting, the psychomotor skills could be tested. Students could be tested on refraction, near add determination, correlation of symptoms to refractive error and determination of the final near prescription for a presbyopic patient or a patient who has a simulated presbyopia. Assessing students’ knowledge about symptoms, epidemiology and expected changes could be accomplished using role playing. This would also be helpful in evaluating a student’s ability to elicit and address a patient’s concerns about changes in vision.
Conclusion
BD’s case of hyperopic presbyopia is similar to many cases that students will see in their careers as optometrists. Early in their training, the testing process and the decision on prescribing seems somewhat mysterious to students, partly because it is so beyond their own visual experience. BD’s case is more interesting than a routine case of presbyopia because of his reaction to his symptoms, both at his first and second visit. Every patient needs the full attention of his clinician to his concerns, and students need guidance in learning how to establish an atmosphere in which patients feel comfortable expressing their problems. Case discussions like this, along with experience in clinical patient care, will help students to become competent clinicians.
References
1. Millodot M. Dictionary of Optometry and Visual Science, Sixth Edition. Boston: Butterworth-Heinemann, 2004, 249.
2. Carlson N, Kurtz D. Clinical Procedures for Ocular Examination, 3rd Edition. New York: McGraw-Hill, 2004, 146-150.
3. Zadnik K. The Ocular Examination, Measurements and Findings. Philadelphia: WB Saunders Company, 1997, 115-117.
4. Werner DL, Press LJ. Clinical Pearls in Refractive Care. Boston: Butterworth-Heinemann, 2002, 139 – 178.
5. Rosenfeld M. “Chapter 15, Clinical Assessment of Accommodation” in Rosenfeld M and Logan N (eds), Optometry, Science, Techniques and Clinical Management, Second Edition. Edinburgh: Elsevier, 2009, 237-239.
6. Newman JM. “Chapter 21, Analysis, Interpretation and Prescription for the Ametropias and Heterophorias” in Benjamin WJ (ed), Borish’s Clinical Refraction. Philadelphia: WB Saunders Company, 1998, 803-806.
7. Fannin TE. “Chapter 21, Presbyopic Addition” in Eskridge JB, Amos J, Bartlett JD. Clinical Procedures in Optometry. Philadelphia: JB Lippincott Company, 1991, 198-205.
8. Grosvenor T. Primary Care Optometry, Fifth Edition. St. Louis, MO: Butterworth Heinemann Elsevier, 2007, 254-256.
9. American Optometric Association Clinical Practice Guideline on Care of the Patient with Presbyopia. St. Louis: AOA. Revised, 2010.
10. Kurtz D. Chapter 7, Presbyopia. Refractive Management of Ametropia. K Brookman, Editor. Boston: Butterworth, 1996.
11. Ettinger ER, Rouse MW. Clinical Decision Making in Optometry. Boston: Butterworth-Heinemann, 1997.
12. Kleinstein RN. Epidemiology of Presbyopia. In Stark L, Obrecht G, eds. Presbyopia: Recent Research and Reviews from the Third International Symposium. New York: Professional Press Books, 1987:12-28.
13. Walline JJ, Zadnik K, Mutti DO. Validity of surveys reporting myopia, astigmatism, and presbyopia. Optom Vis Sci. 1996;73:376-81.
14. Ettinger ER. Professional Communications in Eye Care. Boston: Butterworth-Heinemann, 1994.
15. Lloyd M, Bor R. Communication Skills for Medicine, Second Edition. Edinburgh: Churchill Livingstone, 2004.
16. Moore BD, Ciner EB, Augsberger AR, et al. American Optometric Association Clinical Practice Guideline on Care of the Patient with Hyperopia. St. Louis: AOA. Revised, 2008.
17. Werner DL, Werner W. Presbyopia and mid-life transition. Rev Optom. 1979:July;43.
18. Rouse M, Cooper J, Cotter S, et al. American Optometric Association Clinical Practice Guideline on Care of the Patient with Amblyopia. St. Louis: AOA, 1994.
19. Moore B, Lyons SA, Walline JJ. A clinical review of hyperopia in young children. JAOA. 1998;69(2):88-114.
20. Grosvenor T. Changes in Spherical Refraction During the Adult Years. In Grosvenor T, Flom M, eds. Refraction Anomalies, Research and Clinical Applications. Boston: Butterworth-Heinemann, 1991:131-45
21. Lee KE, Klein BE, Klein R, Wong TY. Changes in refraction over 10 years in an adult population: the Beaver Dam Eye Study. Invest Ophthal Vis Sci. 2002;43:2566-71.