Perceived Enhanced Clinical Readiness for Second-Year Optometry Interns
Fuensanta A. Vera-Diaz, OD, PhD, FAAO, and Catherine Johnson, OD, FAAO
Abstract
In order to meet today’s healthcare environment needs and for our optometry students to play an active role in second-year clinical assignments, student clinical readiness at our institution needed to improve. We made significant changes to the first-year optometric curriculum, specifically, the addition of a more concentrated delivery of didactic and laboratory material and the addition of a summer term that included practice patient experiences. The clinical goal was that students could efficiently complete a routine eye exam up to the point of dilation by the time they enter second-year patient care clinical assignments. Using student and preceptor surveys we evaluated the impact of these changes on our students’ clinical readiness as they entered second-year clinical assignments. Outcomes data showed that student and preceptor perception of students’ confidence and clinical competence increased after the curricular changes were implemented. These findings may indicate increased clinical competency following the curricular changes.
Key Words: optometric education, clinical competency, didactic curriculum, clinical readiness, clinical assignments, clinical training, clinical simulation
Introduction
Healthcare educators increasingly recognize the benefits of early, direct exposure to patient care,1,2 defined as authentic patient contact in a clinical setting that enhances learning.3 Benefits of early exposure to patient care include developing comfort with patients, developing efficient clinical skills, encouraging active learning, making learning more relevant, and reducing difficulty with transition to clinical practice.1,3-6 However, increasing demands on clinicians and clinical settings pose barriers to training through direct patient care.7 The attention and time dedicated to on-site clinical teaching has been eroded by the need for clinicians to take on more administrative tasks while simultaneously being more productive. This leaves clinical preceptors less time to dedicate to teaching basic clinical skills and concepts. At the same time, advances in knowledge and technology have expanded the skills required of optometrists.7,8 In order for optometry students to acquire these skills by the time they graduate, they must become clinically proficient earlier in their student career so they can take most advantage of their clinical experiences as they progress through the curriculum.4,9
During the first year at New England College of Optometry (NECO), students receive the majority of their didactic training on clinical topics in the Principles and Practices of Optometry (PPO) course series. Historically, this course series had included weekly lectures and laboratories throughout the fall and spring semesters of the first year. After a three-month break during the first summer, clinical preceptors noted a significant attrition of clinical skills and knowledge when students returned for the fall semester of second year. Students required a significant “ramp up” refresher period to reach the level they had attained at the end of the first year spring semester. Moreover, internal discussion and anecdotal observations indicated that students needed to be proficient in additional skills prior to entering second year if they were to meet the clinical sites’ demands and play an active role in the clinical setting (e.g., slit lamp evaluation, Goldmann tonometry). These additional skills were not included in the old PPO curriculum.
In response to these needs, the first year PPO curriculum was modified significantly to include a more concentrated delivery of didactic and laboratory material and the addition of a summer term that included practice patient experiences. The purpose of this study was to evaluate the impact of these changes in NECO’s first-year PPO course series on students’ perceived clinical readiness as they entered second-year patient care clinical assignments (Patient Care II). Based on clinical goals identified by NECO’s clinical educators, we defined “clinical readiness” as competence and confidence in performing clinical skills necessary to play an active role in clinic1,2,5,6,9 with the specific goal of completing a routine eye exam up to the point of dilation in an efficient manner in Patient Care II assignments.
Methods
NECO’s optometry doctorate program
NECO’s primary educational program is a four-year Doctorate of Optometry program. Pre-admission requirements include the completion of at least three years of undergraduate preparation with specific coursework. The class size is typically 120-130 students, and students in each class progress through each component of the curriculum at the same time. Students participate in the didactic curriculum during the first three years, with a greater emphasis on general optometric clinical courses (PPO) and basic science courses during the first year and increasing emphasis on more specialized and clinical courses in the second and third years.
NECO’s clinical curriculum begins in first year with an active role in vision screening assignments in addition to observations in various optometry settings (Patient Care I). Students are assigned to clinic at least eight hours per week during their second year (Patient Care II) and at least 12 hours per week during third year (Patient Care III). NECO does not have a large, central clinic dedicated to clinical education. Rather, NECO’s sites for clinical education include a number of smaller affiliated satellites, as well as community health centers, hospitals, private practices and commercial settings.
Study protocol and procedures
Survey instruments (Appendix I; delivered using online tool surverymonkey.com) were developed to evaluate the impact of the PPO track curricular changes, the intervention, on students’ clinical readiness as they entered Patient Care II. The surveys were delivered to all entering Patient Care II students and preceptors during the fall semester in 2014 (old curriculum) and 2015 (new curriculum) by NECO’s Office of Clinical Education. No incentives were provided. Students had participated in Patient Care II clinics for three to four weeks at the point of receiving and answering the survey.
The impact of the intervention was evaluated using three outcome measures that were compared between students enrolled in the old curriculum (Patient Care II in 2014 – OD’17), as controls, and students enrolled in the new curriculum (entered Patient Care in 2015 – OD’18). The specific outcome measures were:
- Level of active participation in patient care in clinic. Table 3 provides a detailed summary of the skills students were expected to be able to perform
- Preceptor and student perception of confidence in clinic
- Preceptor and student perception of competency in clinic
Intervention: specific curriculum changes implemented
The intervention was comprised of significant changes to the first-year optometric curriculum. These changes included expansion of the learning objectives to emphasize clinical readiness, a concentrated delivery of didactic and laboratory material, introduction of skills that previously were not introduced until second year, and the addition of a summer term that included practice patient experiences.
The curriculum changes were made in accordance with NECO’s policies and procedures; a curriculum need was identified, feedback was gathered from didactic and clinical faculty and administration, and a proposal for curriculum change was developed. This proposal was presented to NECO’s Curriculum Committee, comprised of faculty from each department and student representatives. Once vetted and approved by the Curriculum Committee and subsequently the Dean of Academic Affairs, the curriculum changes were implemented. While some of the surveyed preceptors provided input during the curriculum redesign and participated in aspects of implementation, none of the surveyed preceptors was responsible for the development of the new curriculum.
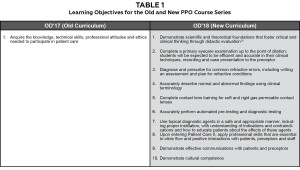
The learning objectives, course structure and content for the old and new PPO course series are summarized in Tables 1 and 2, respectively. In both the old and new curricula, the first-year PPO courses were associated with the clinical course Patient Care I: vision screenings and observations.
Additional details regarding curricular changes are provided in the text.
Topics and skills added to the new curriculum (the intervention) are indicated in bold font.
RE = refractive error; BV = binocular vision; VF = visual field; CL = contact lenses; LV = low vision; EHR = electronic health records; I & R = insertion & removal; GAT = Goldmann applanation tonometry
The overall emphasis of the new PPO course series was clinical readiness. For this purpose, a significant amount of lecture time was allotted to case-based discussion with common clinical scenarios relevant to topics taught in each course of the sequence (e.g., screening scenarios in PPO1).11 These case-based discussions were team-taught, with participation of didactic and clinical faculty. Laboratories were redesigned to be additive, with each skill reinforced in several laboratories throughout the year, increasingly integrated into a typical clinical sequence. These new laboratories also emphasized correlation of findings as well as accurate and efficient performance of procedures and recording. Specific objectives and metrics to monitor student performance were included in each laboratory. In the old curriculum, there was less emphasis on case-based discussion and correlation of findings, and less integration of skills into a typical clinical sequence. No major content topics where removed following these curricular changes. The additions were possible due to reorganization and streamlining of these courses and the addition of the Principles and Practice of Optometry 3 (PPO3) course.
One major change in the new PPO curriculum was the addition of the summer course (PPO3). This course was comprised of seven teaching weeks and was primarily laboratory and clinically based. (Table 2) The PPO3 course included practice patient experience with direct supervision and feedback from clinical preceptors. The purpose of the practice patient experience was to expose student clinicians to naïve patients who are more likely to respond as real patients to the student’s demeanor, instructional sets and test, rather than classmates who are familiar with the testing being performed. Practice patients were also introduced to reduce the “shock value” of seeing real patients in a busy clinical setting.5,6,12
Volunteers were recruited by the students to serve as practice patients for the PPO3 clinical simulations sessions. Each student recruited one patient for week four and one patient for week six of the course. These patients were examined by students other than those who recruited them. Students were provided with specific criteria for the recruitment of practice patients, such as age between 18 to 80 years, corrected vision of 20/40 or better in the best eye, and no relation to optometry (e.g., not an optometrist, optician, technician, optometry student, faculty member). Each student examined a total of five practice patients during his or her clinical simulations sessions. The practice patients were compensated $25 for each two-hour session. Other resources associated to the implementation of this course were exam lanes (one per student), additional clinical preceptors (preceptor:student ratio 3:19) and additional equipment.
In both the old and new curricula, one clinical skills practical exam was administered during the fall (PPO1) and during the spring (PPO2) of first year. A comprehensive clinical skills practical exam with non-optometry presbyopic patients was added during the summer between the first and second year. Table 2 shows details on the topics for each clinical skills exam. Students were required to pass the skills exam in order to progress through the clinical curriculum.
Strong collaboration between the clinical and didactic faculty was key to integrating the PPO courses with the clinical programs. Clinical faculty were integrated as screening preceptors (Patient Care I) and PPO laboratory instructors, with distinct and planned roles. Additionally, tools for student self-learning and opportunities for self-evaluation such as pre-lecture videos, hands-on homework assignments, case assignments, and quizzes were implemented. Alternative teaching approaches utilizing new technology and hybrid teaching were incorporated.
Subjects
All students enrolled in the NECO Patient Care II program in the fall of 2014 (OD’17; n=134; 90 female, 44 male) and fall of 2015 (OD’18; n=125; 90 female, 35 male) were surveyed. All clinical preceptors for the NECO Patient Care II program were surveyed (n=60 in 2014 and n=61 in 2015). A total n=49 preceptors were surveyed both years.
Patient Care II students were assigned to a wide range of clinical settings: NECO affiliated clinics, community health centers, hospitals, private practices and commercial practices. The clinical focus of the majority of these sites was primary eye care, while approximately one third of these sites provided specialized eye care such as low vision, pediatrics or advanced contact lenses. The ratio of clinical preceptors to students was very similar across the settings, with a trend towards a lower ratio of students per preceptor in private practice and commercial settings.
This research followed the tenets of the Declaration of Helsinki. NECO’s Institutional Review Board reviewed and approved this study. Informed consent was not required as participation in the surveys was anonymous.
Data analyses
Statistical analyses were performed using JMP 10.0 (https://www.jmp.com/). Group data for student and preceptor perception of students’ expectations for Patient Care II clinics (Question 1) before (OD’17, fall 2014) and after (OD’18, fall 2015) the implementation of the new curriculum were compared using Wilcoxon signed-rank non-parametric tests (0.05 significance level). Expectations for individual skills for each year were evaluated using Chi Square test for each item (0.05 significance level). Group data for student and preceptor perception of students’ confidence, professionalism and communication skills (Question 2a) and perception of students’ clinical competence (Question 2b) were evaluated using Wilcoxon Rank Sum non-paired, non-parametric tests (0.05 significance level).
Student and preceptor answers to open-ended Question 3 were grouped into the major response categories described in Table 5. Each verbatim comment provided by the subjects was independently coded by the authors and included in one of the major response categories. A subsequent qualitative code analysis was conducted.
Results
The response rate for students was 91/134 (68%) in the fall of 2014 and 112/125 (73%) in the fall of 2015. The response rate for the Patient Care II clinical preceptors online survey was 30/60 (50%) in the fall of 2014 and 35/61 (57%) in the fall of 2015.
Numbers indicate the percentage of respondents who listed that skill as an activity expected to be performed in clinic
Values with * indicate significant difference between student and preceptor surveys in each year (Chi Square test for each item, 0.05 significance level)
Values with ♯ indicate significant difference between 2014 and 2015 in the number of students or preceptors who reported to perform this activity (Chi Square test for each item, 0.05 significance level); these skills and percentage values are also indicated with bold font
Results of the 2014 preceptor survey (Appendix I, Question 4 for preceptors) corroborated initial discussions and anecdotal evidence suggesting that preceptors would be interested in giving second-year students additional patient care responsibilities if they had previously developed those skills. Most preceptors (86% of those who responded) would be interested in giving second-year students additional patient care responsibilities such as performing anterior segment evaluation with slit lamp and Goldmann tonometry. Additionally, preceptors reported a need for students to improve efficiency in conducting a comprehensive exam up to the point of dilation upon entering their second year if they were to be allowed to conduct more independent exams on patients during their Patient Care II assignments. Therefore, the curricular changes described in the methods section were implemented.
The student and preceptor perception of students’ expectations for Patient Care II clinics were compared between the class before (OD’17, fall 2014) and after (OD’18, fall 2015) the implementation of the new curriculum. (Table 3) These data were obtained from Question 1 of the surveys. (Appendix I) A significant improvement in the correlation of preceptors and students expectations for Patient Care II clinical assignments was found for the group of skills surveyed (Wilcoxon Rank, p=0.04).
The specific techniques that were ranked higher in 2015 than 2014 were near refraction in presbyopes, anterior segment evaluation using a slit lamp, undilated fundus evaluation, contact tonometry and patient education. The general expectations of preceptors and students for what activities the students should be able to perform in Patient Care II (Question 1) were higher in 2015 than 2014, (Table 3) even for certain techniques that were not emphasized in the new curriculum, e.g., ophthalmoscopy, or techniques that students had not yet learned in the PPO track, e.g., dilated fundus evaluation using a binocular indirect ophthalmoscope. Preceptors had higher expectations than students both years, but their expectations were closer to students’ in 2015 (cumulative rating preceptors 2014: 44.4, students 2014: 37.0; preceptors 2015: 50.5, students 2015: 44.4).

Numbers indicate average ranking for each question (1-Strongly Disagree, 2-Disagree, 3-Neither Disagree nor Agree, 4-Agree, 5-Strongly Agree)
A higher number indicates a better ranking; items 1 through 8 are relevant to student confidence and attitude (Question 2a); items 9 through 18 are relevant to student competence in clinic (Question 2b)
The student and preceptor perception of students’ confidence and competence in Patient Care II clinics were compared between the class before (OD’17, fall 2014) and after (OD’18, fall 2015) the implementation of the new curriculum. (Table 4)
Items 1 through 8 of Question 2a were related to perception of student confidence and attitudes. Answers to these questions revealed a trend towards student perception of their confidence and attitude being higher than their preceptors’ perception, although this difference was not significant (Wilcoxon Rank Sum, S=-1.8, p=0.78) (mean rating for items 1-8 was 4.17 for 2014 and 4.20 for 2015). No significant changes were found from 2014 to 2015 (Wilcoxon Rank Sum, S=-3, p=0.67).

Numbers indicate the percentage of subjects (students or preceptors) who gave a response that was included in the specific response category (higher numbers indicate that more subjects thought that area or skill needed improvement in order to more effectively participate in Patient Care II clinics)
The categories that improved from 2014 to 2015 are indicated in grey shading
Most technical skills, particularly slit lamp, retinoscopy, subjective refraction and case history, and general confidence in skills and results, improved from 2014 to 2015 based on both student and preceptor perceptions
Note that tonometry was not part of the curriculum in 2014, and fundus evaluation was not part of the curriculum in 2014 or 2015
* Communication with patients refers to general communication, including non-English-speaking patients
** Communication with preceptors includes presentation of cases
§ General exam flow refers to determining order of testing and tests needed for each patient
¶ Refers to technique, accuracy and efficiency
BIO = binocular indirect ophthalmoscope; EMR = electronic medical records
Items 9 through 16 (Question 2b) were related to perception of competence. Answers to these questions revealed that students’ perception of their performance was higher than their preceptors’ perception (Wilcoxon Rank Sum, S=18.5, p=0.026) (mean rating for items 9-16 was 3.52 for 2014 and 3.66 for 2015). Students’ perception of clinical competence significantly improved from 2014 to 2015 (mean difference 0.21, Wilcoxon Rank Sum, S=22.5, p=0.019), whereas there was no significant change in preceptors’ perception of students’ clinical competence between the two years (mean difference 0.08, Wilcoxon Rank Sum, S=8.0, p=0.41). Note that preceptors were aware of the curricular changes and their expectations should have been higher in 2015. Overall analyses of items 9-16 for both students and preceptors showed a significant improvement in perception of competence from 2014 to 2015 (Wilcoxon Rank Sum, S=59, p=0.026).
The percentages of students who gave comments to open-ended Question 3 were 59% (n=54) in 2014 and 76% (n=85) in 2015; the percentages of preceptors who gave comments to this open-ended question were 67% in 2014 and 74% in 2015. This open-ended question yielded insight into how students could be better prepared for Patient Care II clinics. (Table 5) Verbatim answers were classified into major categories that showed that most technical skills, particularly slit lamp, retinoscopy, subjective refraction and case history, improved from 2014 to 2015, based on both students’ and preceptors’ perception. General efficiency was the most commonly reported category for both years, and improved only minimally between 2014 and 2015 according to student and preceptor responses.

Rankings are from most useful (1) to least useful (12)
A lower number indicates a better ranking
The three top-ranked activities are indicated in bold font (laboratories, clinical skills exams and practice patient experiences were ranked as most useful, and written exams were ranked as least useful)
When asked to rank the usefulness of the various components of the PPO courses in preparing students for clinic (student Question 5), students consistently ranked PPO laboratories as the most useful activity. Clinical skills practical exams, regular lectures and Patient Care I assignments (vision screenings) followed laboratories in the ranking of useful activities. (Table 6) In 2015, students had two new activities in the new summer term: practice patient experiences, rated highly, and clinical readiness seminars, rated lower than clinical skills exams, lectures, Patient Care I assignments and seminars where clinical cases were discussed. (Table 6)
Discussion
The main changes in the PPO curriculum were a more concentrated delivery of didactic and laboratory material and the addition of a summer term between first year and the fall of second year that included practice patient experiences. These modifications may have contributed to the perceived improvement in clinical readiness of OD’18 students entering their second-year clinical rotations. Studies have shown that early patient encounters with direct supervision from preceptors, one-on-one clinical skills training, and timely feedback provide benefits to clinical skills training and non-analytical reasoning skills,1,13 as well as increased comfort with clinical settings and patients1 and motivation.5 In addition, simulated patient encounters with feedback are known to result in improved student-patient communication.14
With implementation of the new curriculum, both the student and preceptor surveys showed that students had begun to take a more active role in patient care during their clinical assignments, including less observation of preceptors and upper-year students and less automated pre-testing. This is likely related to changes in students’ skill set. Students were able to acquire basic proficiency in individual clinical techniques required to complete a primary care comprehensive eye exam, up to the point of instilling dilation drops, prior to starting clinical assignments in the fall of their second year. Skills such as slit lamp evaluation and contact tonometry were added earlier in the curriculum. Also, students were able to gain more experience with visual field testing and other supplemental tests, which preceptors had previously identified as being helpful for efficiency in their clinics, prior to entering second-year clinics. Additionally, students were introduced to essential clinical skills related to communication, patient interaction and clinical reasoning.
Student and preceptor expectations also converged after implementation of the new curriculum. Particularly, students’ perception of their clinical competence increased after the curriculum changes, which was also reflected in the expectations of their role in the clinic. While preceptors’ expectations for students remained stable for some skills from 2014 to 2015, student expectations improved for most skills, notably: near refraction, undilated anterior segment evaluation, drop instillation, contact tonometry, binocular vision testing, automated visual field testing, optical coherence tomography testing and fundus photography. Each new skill that students were expected to perform in clinic promoted their ability to participate in a clinical setting, at a level similar to that that of past students entering their third year rather than their second year. This, in turn, allowed second-year students to be placed in a wider array of clinical settings, and for upper-year students to be placed in settings where they could gain more advanced training.15
Of note, many of the skills identified as deficient in 2014 were addressed after the curriculum changes, as shown in open-ended Question 3. In particular, most technical skills (slit lamp, retinoscopy, subjective refraction and case history) were identified by students and preceptors as improved from 2014 to 2015. There was an improvement in student efficiency using electronic medical/health records systems, although this is an area that needs to improve further. Note that tonometry was not part of the curriculum in 2014 and fundus evaluation was not part of the curriculum in 2014 or 2015. These areas do not appear to be deficient, probably because they were not perceived as essential for participation in Patient Care II clinical assignments.
After the implementation of the new curriculum, students and preceptors appeared less concerned about students’ skills and more about general exam efficiency, flow and communication, which are more advanced aspects of clinical performance. Interestingly, preceptors’ perception of students’ communication with patients and exam flow seemed to improve in 2015, but students’ perception did not. Preceptors’ perception of students’ ability to communicate with preceptors was poorer than that of students. General efficiency, the most commonly reported category for both years, improved only minimally between 2014 and 2015 by students and preceptors.
The main challenges encountered in the implementation of the new curriculum were related to the recruitment and scheduling of practice patients. Students requested that future practice patient recruitment be coordinated, recruited and scheduled by the College. Other challenges were related to the student:preceptor ratio in clinical simulations and laboratories, which made implementation of student performance evaluation rubrics and clinical readiness seminars difficult. In spite of these challenges, mostly practice patient experiences were highly ranked in the list of usefulness in preparing students for their clinical assignments. (Table 6) Laboratories and clinical skills exams were ranked as the most useful activities.
One limitation of this study was the timing of delivery of the survey, which was administered three weeks into the fall academic semester. Given that most students are assigned to clinic one day per week in their second year, students were still acquiring familiarity with the clinical setting, and preceptors were still acquiring familiarity with their students. Thus, the results reflect perceptions of expectations, competence and confidence rather than an objective assessment of these factors. However, these perceptions are important in designing a curriculum that provides the foundation for a comfortable yet motivating clinical training environment. In the future, surveys or other measures of student performance will be needed to assess the long-term impact of these curricular changes.
Conclusion
A concentrated delivery of didactic and laboratory material during the first year of optometry school, including the addition of a summer term that included practice patient experiences, may have improved student clinical readiness. This enhanced students’ confidence and perception of their competence, and it aided their ability to meet the expectations of their preceptors and the needs of the student clinics. As a consequence, a more robust clinical experience could be achieved. Further study is needed to assess the long-term impact of these curricular changes on student performance and perceptions.
Acknowledgments
This study was supported in part by a Starter Grant for Educational Research from the Association of Schools and Colleges of Optometry. Funding for the grant was provided by Johnson & Johnson Vision Care, Inc.
We are grateful to Erik Weissberg, OD, and Beth Harper, OD, from New England College of Optometry’s Office of Clinical Education, for their helpful insights in the creation of the surveys, and Cameron MacMartin for delivery of the surveys. We are thankful to Li Deng, MS, MA, PhD, Associate Professor of Biostatistics at the College, for her support with data and statistical analyses.
References
1. Wenrich M, Jackson M, Wolfhagen I, Ramsey P, and Scherpbier A. What are the benefits of early patient contact? A comparison of three preclinical patient contact settings. BMC Med Educ. 2013;13:80.
2. Littlewood S, Ypinazar V, Margolis S, Schrpbier A, Spencer J, Dornan T. Early practical experience and the social responsiveness of clinical education: systematic review. Br Med J. 2005;331:387–91.
3. Dornan T, Tan N, Boshuizen H, Gick R, Isba R, Mann K, Scherpbier A, Spencer J, Timmins E. How and what do medical students learn in clerkships? Experience based learning (ExBL). Adv Health Sci Educ. 2014;19(5):721–49.
4. Yardley S, Littlewood S, Margolis S, Scherpbier A, Metsemakers J. What has changed in the evidence for early experience? Update of BEME systematic review. Med Teach. 2010;32:740–6.
5. Godfrooji M, Diemers A, Scherpbier A. Students’ perceptions about the transition to the clinical phase of a medical curriculum with preclinical patient contacts; a focus group study. BMC Med Educ. 2010;10:28.
6. Diemers A, Dolmans D, Verwijnen M, Heineman E, Scherpbier A. Students’ opinions about the effects of preclinical patient contacts on their learning. Adv Health Sci Educ. 2008;13:633–47.
7. American Optometric Association (AOA) [Internet]. The state of the optometric profession. 2013 [cited 2016 Feb 9]. Available from: https://www.aoa.org/Documents/news/state_of_optometry.pdf.
8. Association of Schools and Colleges of Optometry (ASCO) [Internet]. Optometry: A Career Guide. 2013. [cited 2016 Feb 9]. Available from: https://www.opted.org/wp-content/uploads/2013/03/EyesHaveIt_CareerGuide.pdf.
9. Whipple M, Barlow C, Smith S, Goldstein E. Early introduction of clinical skills improves medical student comfort at the start of third year clerkships. Acad Med. 2006;81(10):S40–3.
10. Horsley T, Hyde C, Santesso N, Parkes J, Milne R, Stewart R. Teaching critical appraisal skills in health care settings (Review). Cochrane Database Syst Rev. 2011;9(11):CD001270.
11. Wangensteen S, Johansson I, Björkström M, Björkström G. Newly graduated nurses perception of competence and possible predictors: a cross-sectional survey. J Prof Nurs. 2012;28(3):170–81.
12. Small R, Soriano R, Chietero M, Quintana J, Parkas V, Koestler J. Easing the transition: medical students’ perceptions of critical skills required for the clerkships. Educ Health. 2008;21(3):192.
13. Ottenheijm R, Zwieterine P, Scherpbier A, Metsemakers J. Early student-patient contacts in general practice: an approach based on educational principles. Med Teach. 2008;30:802–8.
14. Anderson H, Young J, Marrelli D, Black R, Lambreghts K, Twa M. Training students with patient actors improves communication: a pilot study. Optom Vis Sci. 2014;91(1):121–8.
15. Windish D, Paulman P, Goroll A, Bass E. Do clerkship directors think medical students are prepared for the clerkship years? Acad Med. 2004;79:56–61.